Defining the Problem
Most healthcare organizations rely on the electronic health record (EHR) as the central system for clinical documentation, patient information, and billing. EHRs are effective at managing clinical data and reimbursement workflows, but they are not designed to function as operational coordination tools.
To address staffing and coverage needs, many organizations adopt dedicated scheduling platforms. These tools are often built for large, centralized health systems with standardized roles, stable staffing models, and dedicated administrative teams. As a result, they tend to require significant onboarding, configuration, and training before they can be used effectively at the frontline level.
For smaller healthcare organizations—such as community clinics, safety-net practices, and multi-site primary care settings—these assumptions often do not hold.
Where Equity Enters the Equation
Care settings that serve underserved populations frequently operate under different conditions:
smaller administrative teams
higher staff turnover
variable staffing patterns
limited time for extended onboarding or system customization
frequent day-to-day adjustments driven by patient needs and resource constraints
When scheduling tools are designed primarily for large enterprises, smaller organizations are often left to adapt systems that do not fully reflect their operational reality. In practice, this leads many teams to rely on spreadsheets, shared calendars, email threads, and informal communication layered on top of existing systems.
These workarounds are not signs of poor planning. They reflect the flexibility and resilience required to keep care accessible in constrained environments.
How the Work Began
This project grew out of managing provider and support staff schedules in a clinical setting and responding to day-to-day feedback from providers and staff.
What I did
I sent weekly excel sheets to all relevant staff and providers.
Managed coverage changes and day-of-care adjustments as they occurred. I would send emails, teams messages, or text when changes occured.
What feedback revealed
Providers wanted a quick way to see where they were assigned and who they were working with.
Staff needed clearer visibility into changes as they happened.
Static documents and email updates were hard to reference in real time.
Key insight
Mobile access mattered. Providers consistently noted that being able to view their schedule from a phone would change how easily they could orient their day.
What I explored next
To test how operational information might be surfaced more clearly, I created early exploratory prototypes using AI-assisted design tools (including Bolt). These prototypes were informed by provider and staff feedback and were not used in live operations.
Framing the Scheduling Environment
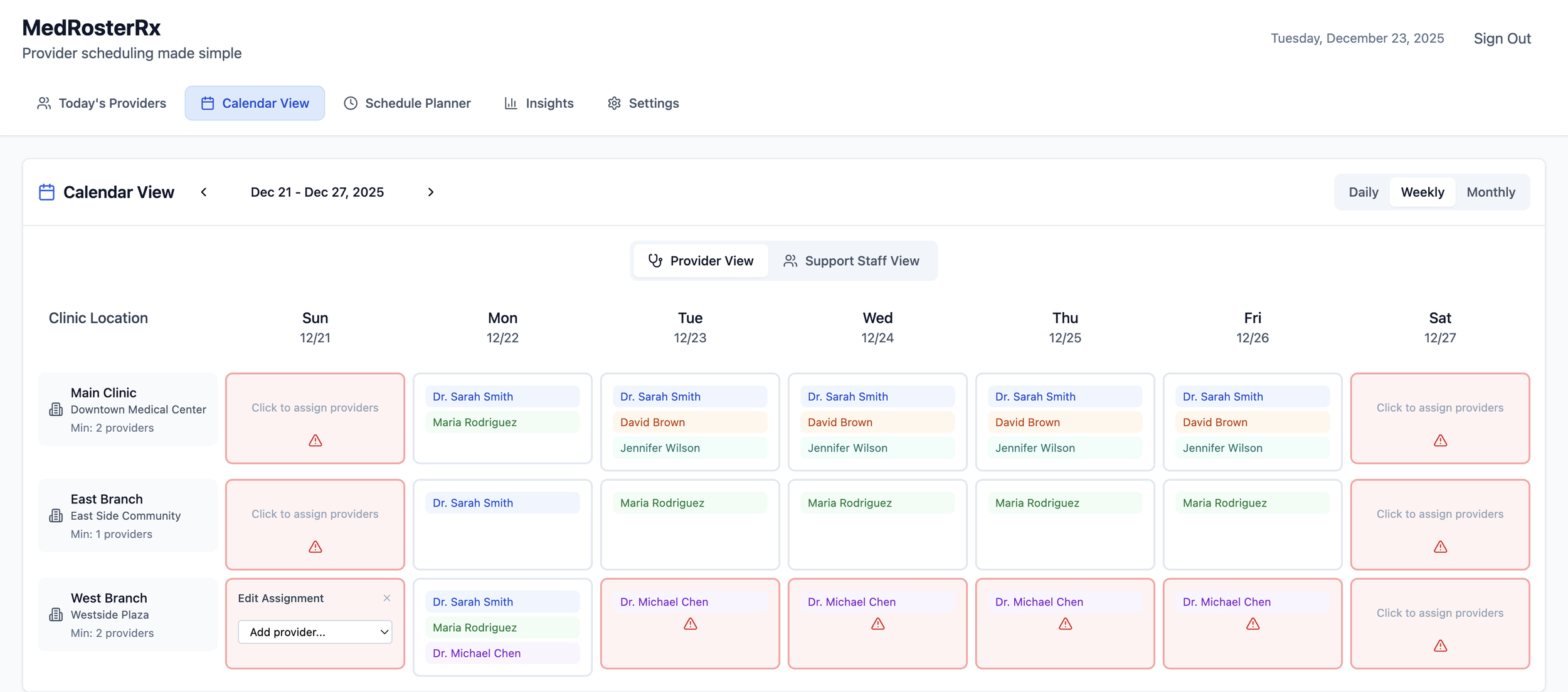
One way I explored alignment between operational scheduling and the EHR was by first modeling the environment in which scheduling actually occurs. This meant defining clinic locations, providers, and support staff who worked within them, establishing a basic representation of the system before attempting to generate schedules.
Once that structure was in place, I introduced the concept of provider cadences. Rather than constructing schedules day by day, I treated a provider’s schedule as a repeating work pattern that already existed clinically. An administrator could define that pattern once, such as a provider working Mondays, Wednesdays, and Fridays, and apply it across a defined time period.
By anchoring scheduling to these predefined environments and patterns, administrators were no longer repeatedly translating the same information from the EHR into operational tools. The operational schedule reflected the clinical reality by default, with manual changes only required when the underlying pattern changed.
The goal was not automation for its own sake, but consistency. Explicitly modeling clinics, providers, and their predictable work patterns reduced rework, preserved alignment with the EHR, and made schedules easier to maintain and extend over.
Real Time Flexibility was a Requirement
Although the cadences were made in advance. As an administrator I needed the ability to drag and drop providers to locations and very easily change projected weekly views. In my prototyping nothing couldn’t be changed in real time. A problem that arose was once the cadence was “broken” it no longer was associated with the rest of the dates in the original string. This increased the risks of accidental duplications.
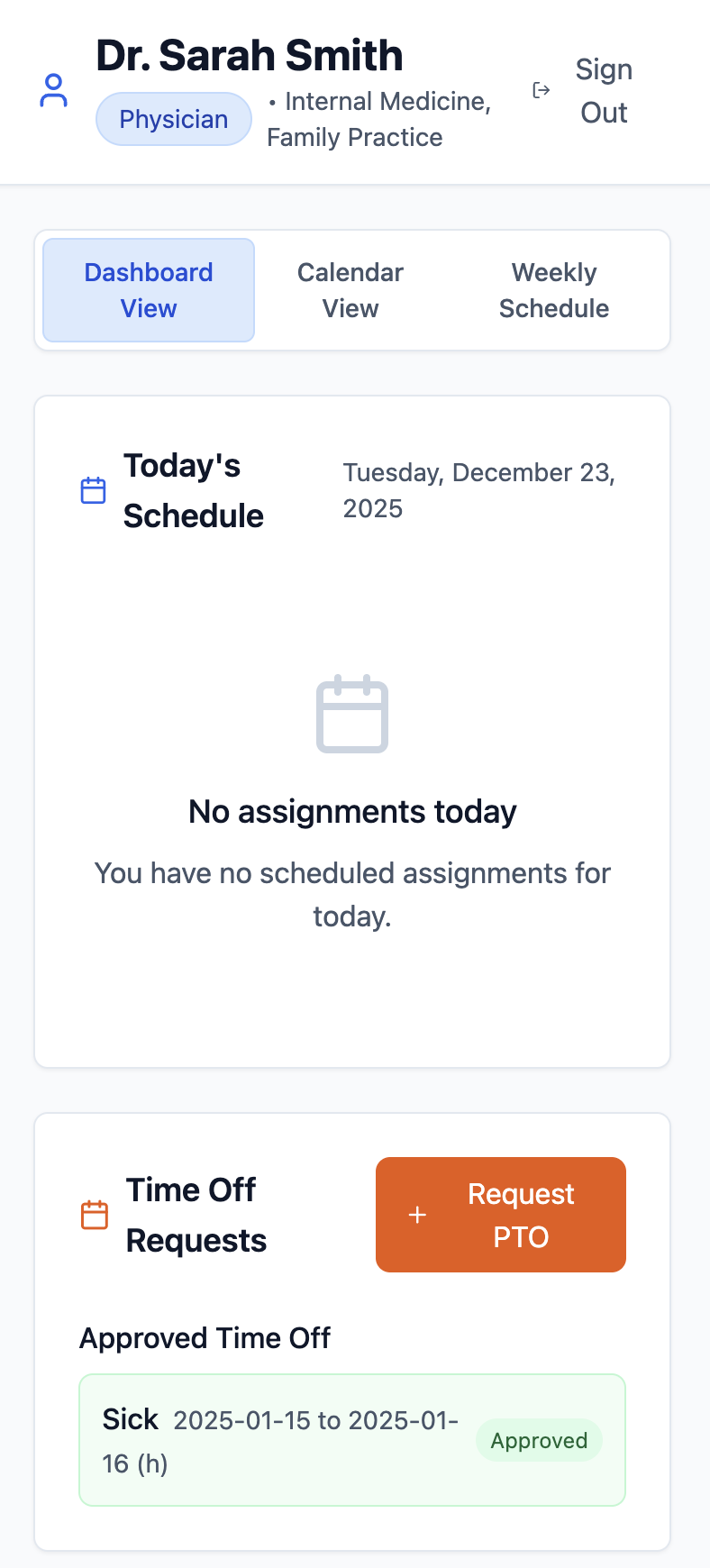
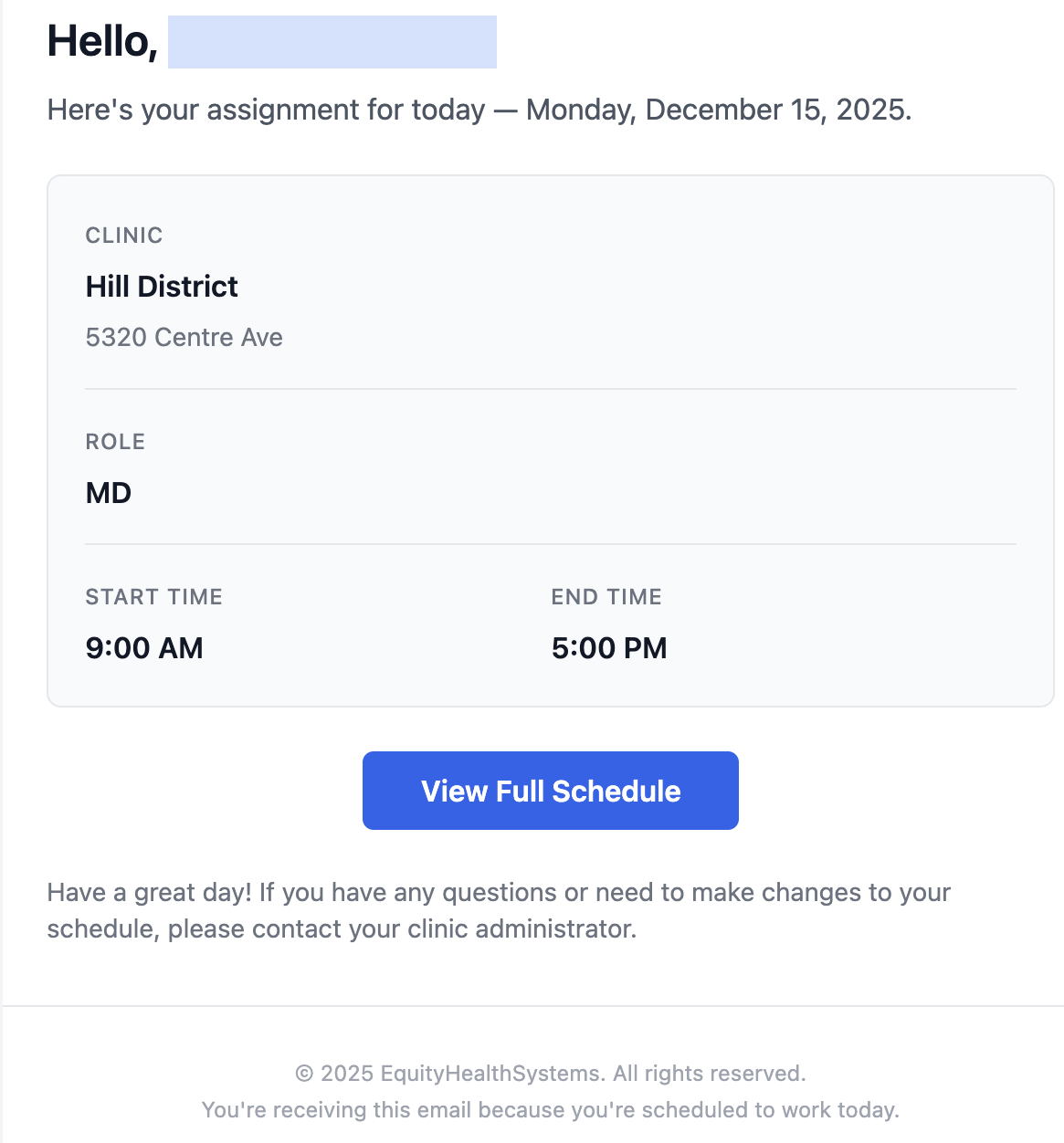
Mobile Visibility is a Point of Need
Another area I explored was mobile visibility of the daily schedule. In practice, schedules are most often needed when staff are away from a desk, responding to last-minute changes, or trying to quickly confirm coverage during the day. In those moments, static spreadsheets or desktop-only tools break down.
To address this, schedule access was designed around how staff actually receive information. Providers and support staff could receive an email containing a direct link to their daily schedule, formatted to work reliably on a mobile device. Opening the link required no special setup and allowed individuals to quickly confirm where they were assigned and who else was on site.
This approach reduced the need for follow-up calls, screenshots, or manual confirmations. When the schedule was easy to reference in real time, coordination became simpler and less error-prone, particularly during same-day changes.
The emphasis again was not novelty, but reliability. By ensuring the schedule was accessible at the point of need through a simple mobile-friendly link, operational communication improved without introducing additional workflow burden.
Insights from a Scheduling System Pilot at a Multi-Site Community Health Center
The goal of the pilot was not to introduce a new scheduling system wholesale, but to test whether clearer structure and visibility around daily provider coverage could reduce manual coordination and scheduling friction for clinical and administrative staff.
Pilot focus
How provider schedules could be structured to reflect existing clinical patterns while remaining visible and reliable enough that providers did not need to cross-check the EHR for daily assignments
How different schedule views, particularly weekly and calendar-based layouts, supported providers and administrators in anticipating coverage and identifying gaps earlier
How the scheduling needs of support staff differed from those of providers, given their multiple roles and task-based assignments, and why a single scheduling model may not serve both effectively
What additional operational insight could be gained by organizing and extracting scheduling data in ways that extend beyond the views and metrics typically available in the EHR
Observations and takeaways
One observation from the pilot was that when support staff were not explicitly included in the schedule, some providers reverted to referencing the EHR to confirm their daily assignments. This reinforced how important it was for operational schedules to reflect the full care team, not just provider coverage, in order to remain a reliable source of truth.
Calendar-based views proved especially valuable for providers. Being able to see assignments laid out visually and to look further into the future helped providers orient themselves and reduced uncertainty around upcoming clinic days. These views aligned more closely with how providers naturally think about their schedules.
For administrative staff, weekly and calendar views made it significantly easier to manage provider coverage across sites. Seeing schedules over a longer time horizon helped identify gaps and inconsistencies earlier, rather than discovering issues on the day of clinic.
Adoption among support staff was more challenging. Unlike providers, support staff often fill multiple roles across locations and are scheduled through a different operational process that focuses on task coverage rather than fixed clinical sessions. This made it harder to represent their work using the same structures designed for provider scheduling and highlighted the need for distinct approaches to support and provider scheduling.
Finally, the pilot highlighted the potential value of extracting and organizing scheduling data in ways that current EHRs do not support well. Having the ability to generate statistics, summaries, and alternative views of the schedule created opportunities for better planning and operational insight beyond what standard EHR scheduling tools provide.
Interact.
Explore a working provider and support staff scheduling tool designed to bring clarity to daily clinic operations.
Demo environment only. No data is saved.
Curious to explore ideas, build responsibly, or learn together? Thoughtful conversations are always welcome..
Prefer email?
wgenerett@equityhealthsystems.com